Kidney failure definition
- Kidneys are the organs that filter waste products from the blood. They are also involved in regulating blood pressure, electrolyte balance, and red blood cell production in the body.
- Symptoms of kidney failure are due to the build-up of waste products and excess fluid in the body that may cause weakness, shortness of breath, lethargy, swelling, and confusion. Inability to remove potassium from the bloodstream may lead to abnormal heart rhythms and sudden death. Initially kidney failure may cause no symptoms.
- There are numerous causes of kidney failure, and treatment of the underlying disease may be the first step in correcting the kidney abnormality.
Facts
- Some causes of kidney failure are treatable and the kidney function may return to normal. Unfortunately, kidney failure may be progressive in other situations and may be irreversible.
- The diagnosis of kidney failure usually is made by blood tests measuring BUN, creatinine, and glomerular filtration rate (GFR).
- Treatment of the underlying cause of kidney failure may return kidney function to normal. Lifelong efforts to control blood pressure and diabetes may be the best way to prevent chronic kidney disease and its progression to kidney failure. As we age, kidney function gradually decreases over time.
- If the kidneys fail completely, the only treatment options available may be dialysis or transplant.
What Is Kidney Disease? What Are the Symptoms?
Kidney disease refers to conditions and problems with the kidneys and their function. Signs and symptoms of kidney disease may vary depending upon the type; however, common non-specific symptoms of chronic kidney disease include:
- Loss of appetite
- Puffiness around the eyes
- Fatigue
- Dry, itcy
- Problems sleeping
What are the kidneys? Where are they located?
The kidneys play key roles in body function, not only by filtering the blood and getting rid of waste products, but also by balancing the electrolyte levels in the body, controlling blood pressure, and stimulating the production of red blood cells.
The kidneys are located in the abdomen toward the back, normally one on each side of the spine. They get their blood supply through the renal arteries directly from the aorta and send blood back to the heart via the renal veins to the vena cava. (The term “renal” is derived from the Latin name for kidney.)
What do the kidneys do?
When blood flows to the kidney, sensors within specialized kidney cells regulate how much water to excrete as urine, along with what concentration of electrolytes. For example, if a person is dehydrated from exercise or from an illness, the kidneys will hold onto as much water as possible and the urine becomes very concentrated. When adequate water is present in the body, the urine is much more dilute, and the urine becomes clear. This system is controlled by renin, / a hormone produced in the kidney that is part of the fluid and blood pressure regulation systems of the body.
Erythropoietin
Kidneys are also the source of erythropoietin in the body, a hormone that stimulates the bone marrow to make red blood cells. Special cells in the kidney monitor the oxygen concentration in blood. If oxygen levels fall, erythropoietin levels rise and the body starts to manufacture more red blood cells.
Urine that is made by each kidney flows through the ureter, a tube that connects the kidney to the bladder. Urine is stored within the bladder, and when urination occurs, the bladder empties urine through a tube called the urethra.
What causes kidney failure?
Kidney failure may occur from an acute situation that injures the kidneys or from chronic diseases that gradually cause the kidneys to stop functioning.
In acute renal failure, kidney function is lost rapidly and can occur from a variety of insults to the body. Since most people have two kidneys, both kidneys must be damaged for complete kidney failure to occur. Fortunately, if only one kidney fails or is diseased it can be removed, and the remaining kidney may continue to have normal kidney (renal) function. If a both patient’s kidneys are injured or diseased, a donor kidney(s) may transplanted.
The list of causes of kidney failure is often categorized based on where the injury has occurred.
Prerenal causes (pre=before + renal=kidney) causes are due to decreased blood supply to the kidney. Examples of prerenal causes of kidney failure are:
- Hypovolemia (low blood volume) due to blood loss
- Dehydration from loss of body fluid (for example, vomiting, diarrhea, sweating, fever)
- Poor intake of fluids
- Medication, for example, diuretics (“water pills”) may cause excessive water loss
- Abnormal blood flow to and from the kidney due to obstruction of the renal artery or vein.
What causes acute kidney failure?
Renal causes of kidney failure (damage directly to the kidney itself) include:
Sepsis: The body’s immune system is overwhelmed from infection and causes inflammation and shutdown of the kidneys. This usually does not occur with simple urinary tract infections.
Medications: Some medications are toxic to the kidney including:
- Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen (Advil, Motrin, and others), and naproxen (Aleve, Naprosyn)
- Antibiotics like aminoglycosides gentamicin (Garamycin), tobramycin
- lithium (Eskalith, Lithobid)
- Iodine-containing medications such as those injected for radiology dye studies
Rhabdomyolysis: In rhabdomyolysis there is significant muscle breakdown in the body, and the damaged muscle fibers clog the filtering system of the kidneys. Massive muscle injury may occur because of trauma, crush injuries, and burns. Some medications used to treat high cholesterol may cause rhabdomyolysis.
Multiple myeloma
Acute glomerulonephritis or inflammation of the glomeruli, the filtering system of the kidneys. Many diseases can cause this inflammation including:
- Systemic lupus erythematosus
- Wegener’s granulomatosis
- Goodpasture syndrome.
Hemolytic uremic syndrome: This condition results from abnormal destruction of red blood cells. It most often occurs in children after certain infections, but also may be caused by medications, pregnancy, or can occur for unknown reasons.
Postrenal kidney failure causes
Post renal causes of kidney failure (post=after + renal= kidney) are due to factors that affect outflow of the urine:
- Obstruction of the bladder or the ureters can cause back-pressure be
 cause the kidneys continue to produce urine, but the obstruction acts like a dam, and urine backs up into the kidneys. When the pressure increases high enough, the kidneys are damaged and shut down.
cause the kidneys continue to produce urine, but the obstruction acts like a dam, and urine backs up into the kidneys. When the pressure increases high enough, the kidneys are damaged and shut down. - Prostatic hypertrophy or prostate cancer may block the urethra and prevents the bladder from emptying.
- Tumors in the abdomen that surround and obstruct the ureters.
- Kidney stones. Usually, kidney stones affect only one kidney and do not cause kidney failure. However, if there is only one kidney present, a kidney stone may cause the remaining kidney to fail.
What causes chronic kidney failure?
Chronic renal failure develops over months and years. The most common causes of chronic renal failure are related to
- poorly controlled diabetes,
- poorly controlled high blood pressure, and
- chronic glomerulonephritis.
Less common causes of chronic renal failure include:
- Polycystic kidney disease
- Reflux nephropathy (damage caused by urine backflow from the bladder into the ureters and kidney)
- Nephrotic syndrome
- Alport’s disease
- Interstitial nephritis
- Kidney stones
- Prostate disease
What are the signs and symptoms of kidney failure?
Initially, kidney failure may be not produce any symptoms (asymptomatic). As kidney function decreases, the symptoms are related to the inability to regulate water and electrolyte balances, clear waste products from the body, and promote red blood cell production.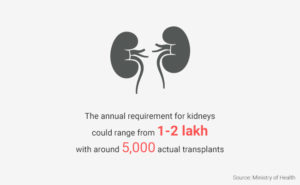
If unrecognized or untreated, the following symptoms of kidney failure may develop into life-threatening circumstances.
- Lethargy
- Weakness
- Shortness of breath
- Generalized swelling (edema)
- Generalized weakness due to anemia
- Loss of appetite
- Lethargy
- Fatigue
- Congestive heart failure
- Metabolic acidosis
- High blood potassium (hyperkalemia)
- Fatal heart rhythm disturbances (arrhythmias) including ventricular tachycardia and ventricular fibrillation
- Rising urea levels in the blood (uremia) may lead to brain encephalopathy, pericarditis(inflammation of the heart lining), or low calcium blood levels (hypocalcemia)
Does kidney failure cause pain?
Kidney failure in itself does not cause pain. However, the consequences of kidney failure may cause pain and discomfort in different parts of the body.
Amyloid proteins
Normal functioning kidneys filter amyloid (a protein) from the blood stream. In kidney failure amyloid proteins in the blood rise, and can separate and clump together forming amyloid deposits into a variety of tissue and organs, including joints and tendons. This can result in symptoms of:
- joint stiffness,
- pain, and
- swelling.
Procedure related pain
- Patients who are on dialysis may have discomfort when on the dialysis machine.
Underlying chronic disease pain
- Pain is often a consequence of the underlying chronic disease that led to kidney failure, for example:
- People with poorly controlled diabetes may develop diabetic neuropathy pain.
- People who have peripheral vascular disease also may have pain in their extremities, and may develop claudication (leg pain that occurs with walking).
How is kidney failure diagnosed?
Often, a patient is seen for another medical condition and the diagnosis of kidney failure is a consequence of the patient’s disease or injury. In patients with chronic kidney disease due to diabetes, high blood pressure, or another related medical condition his or her medical care team most likely monitors kidney function as part of the his or her routine long-term medical care plan.
Blood tests
Diagnosis of kidney failure can be confirmed by blood tests such as BUN, creatinine, and GFR; that measure the buildup of waste products in the blood.
Urine tests
Urine tests may be ordered to measure the amount of protein, detect the presence of abnormal cells, or measure the concentration of electrolytes.
Other tests
Other tests are used to diagnose the type of kidney failure such as:
- Abdominal ultrasound
- Kidney biopsy
What is the treatment for kidney failure?
Prevention is always the goal with kidney failure. Chronic diseases such as hypertension (high blood pressure) and diabetes are devastating because of the damage that they can do to kidneys and other organs. Lifelong diligence is important in keeping blood sugar and blood pressure within normal limits. Specific treatments depend upon the underlying diseases.
Once kidney failure is present, the goal is to prevent further deterioration of renal function. If ignored, the kidneys will progress to complete failure, but if underlying illnesses are addressed and treated aggressively, kidney function can be preserved, though not always improved.
Diet
Diet is an important consideration for those with impaired kidney function. Consultation with a dietician may be helpful to understand what foods may or may not be appropriate.
In this state of impaired kidney function, the kidneys cannot easily remove excess water, salt, or potassium from the blood, so foods high in potassium salt substitutes may need to be consumed in limited quantities. Examples of potassium rich foods include:
- Bananas
- Apricots
- Cantaloupe
- Sweet potatoes
- Yogurt
- Spinach
- Avocados
Phosphorus is a forgotten chemical that is associated with calcium metabolism and may be elevated in the body in kidney failure. Too much phosphorus can leech calcium from the bones and cause osteoporosis and fractures. Examples of foods and beverages high in phosphorus include:
- Milk
- Cheese
- Nuts
- Dark cola drinks
- Canned iced teas
- Yogurt
- Organ meets
- Sardines
- Oysters
- Baked beans
- Black beans
- Lentils
- Kidney beans
- Soy beans
- Bran cereals
- Caramels
- Whole grain products
Medications
Different classes of medications may be used to help control some of the issues associated with kidney failure including:
- Phosphorus-lowering medications, for example, calcium carbonate (Caltrate), calcitriol (Rocaltrol), and sevelamer (Renagel)
- Red blood cell production stimulation, for example, erythropoietin, darbepoetin (Aranesp)
- Red blood cell production (iron supplements)
- Blood pressure medications
- Vitamins
Once the kidneys become fail completely, then treatment options are limited to dialysis or kidney replacement by transplant.
Dialysis and Hemodialysis
Dialysis cleanses the body of waste products in the body by use of filter systems. There are two types of dialysis, 1) hemodialysis, and 2) peritoneal dialysis.
Hemodialysis uses a machine filter called a dialyzer or artificial kidney to remove excess water and salt, to balance the other electrolytes in the body, and to remove waste products of metabolism. Blood is removed from the body and flows through tubing into the machine, where it passes next to a filter membrane. A specialized chemical solution (dialysate) flows on the other side of the membrane. The dialysate is formulated to draw impurities from the blood through the filter membrane. Blood and dialysate never touch in the artificial kidney machine.
For this type of dialysis, access to the blood vessels needs to be surgically created so that large amounts of blood can flow into the machine and back to the body. Surgeons can build a fistula, a connection between a large artery and vein in the body, usually in the arm, that allows a large amount of blood flow into the vein. This makes the vein swell or dilate, and its walls become thicker so that it can tolerate repeated needle sticks to attach tubing from the body to the machine. Since it takes many weeks or months for a fistula to mature enough to be used, significant planning is required if hemodialysis is to be considered as an option.
If the kidney failure happens acutely and there is no time to build a fistula, special catheters may be inserted into the larger blood vessels of the arm, leg, or chest. These catheters may be left in place for weeks. In some diseases, the need for dialysis will be temporary, but if the expectation is that dialysis will continue for a prolonged period of time, these catheters act as a bridge until a fistula can be planned, placed, and matured.
Dialysis treatments normally occur three times a week and last a few hours at a time. Most commonly, patients travel to an outpatient center to have dialysis, but home dialysis therapy is becoming an option for some.
Outpatient dialysis is available on some cruise ships. They are equipped with dialysis machines with trained health care professionals ready to care for those with kidney failure while traveling.
Peritoneal dialysis
Peritoneal dialysis uses the lining of the abdominal cavity as the dialysis filter to rid the body of waste and to balance electrolyte levels. A catheter is placed in the abdominal cavity through the abdominal wall by a surgeon. It is expected to remain in place for the long-term. The dialysis solution is then dripped in through the catheter and left in the abdominal cavity for a few hours after which it is drained out. During that time, waste products leech from the blood flowing through the lining of the abdomen (peritoneum), and attach themselves to the fluid that has been instilled by the catheters. Often, patients instill the dialysate fluid before bedtime, and drain it in the morning.
There are benefits and complications for each type of dialysis. Not every patient can choose which type he or she would prefer. The treatment decision depends on the patient’s illness and their past medical history along with other issues. Usually, the nephrologist (kidney specialist) will have a long discussion with the patient and family to decide what will be the best option available.
Dialysis is life saving. Without it, patients whose kidneys no longer function would die relatively quickly due to electrolyte abnormalities and the buildup of toxins in the blood stream. Patients may live many years with dialysis but other underlying and associated illnesses often are the cause of death.
Kidney transplantation
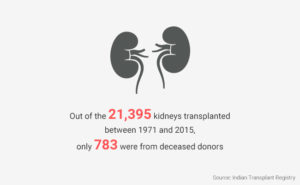
If kidney failure occurs and is non-reversible, kidney transplantation is an alternative option to dialysis. and If the patient is an appropriate candidate, the healthcare professional and nephrologist will contact an organ transplant center to arrange evaluation to see whether the patient is suitable for this treatment. Moreover, the search for a donor begins. Sometimes, family members have compatible tissue types and, if they are willing, may donate a kidney.
Not all hospitals are capable of performing kidney transplants. The patient may have to travel to undergo their operation. The most successful programs are those that do many transplants every year.
While kidney transplants have become more routine, they still carry some risk. The patient will need to take anti-rejection medications that reduce the ability of the immune system to fight infection. The body can try to reject the kidney or the transplanted kidney may fail to work. As with any operation, there is a risk of bleeding and infection.
Kidney transplants may provide better quality of life than dialysis. After one year, 95% of transplanted kidneys are still functioning and after five years, the number is 80%. It seems that the longer a patient is on dialysis, the shorter the life of the transplanted kidney.
If the transplanted kidney fails, the alternative is another kidney transplant or a return to dialysis.
What is the prognosis for someone with kidney failure?
The outlook for kidney failure depends upon the underlying condition that caused it. Kidney function may return to normal, especially if it is due to an acute obstruction. & that obstruction is relieved. Other causes of decreased kidney function leading to kidney failure are due to underlying disease & occur slowly over time.
Prevention is the best chance to maintain kidney function, and controlling high blood pressure and diabetes over a lifetime can decrease the potential for progressive kidney damage. Chronic kidney failure may be managed by to help monitor electrolyte and waste product levels in the bloodstream. Major abnormalities can be life threatening. and treatment options may be limited to dialysis or transplant.